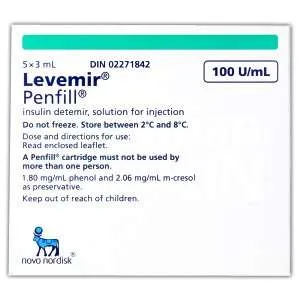
Levemir PenFill Cartridges (100 Units/mL) Description
Levemir Penfill cartridges are designed to be used with Novo Nordisk insulin delivery systems and NovoFine or NovoTwist needles.
1 ml of the solution contains 100 units insulin detemir (equivalent to 14.2 mg). 1 cartridge contains 3 ml equivalent to 300 units. 3 ml solution in cartridge (type 1 glass) with a plunger (bromobutyl) and a rubber closure (bromobutyl/polyisoprene).
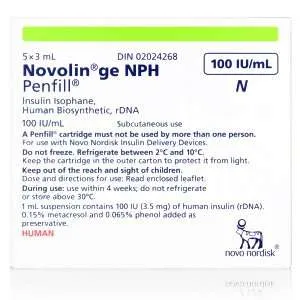
If you are treated with Levemir Penfill and another insulin Penfill cartridge, you should use two insulin delivery systems, one for each type of insulin.
The Levemir PenFill Cartridge contains insulin detemir, a modern analog used to treat blood glucose levels in children (age one year and above), adolescents, and adults with diabetes. Please note, the cartridge cannot be refilled.
Levemir is a long-acting insulin that provides a long and steady glucose-lowering action that begins 3-4 hours after injection and lasts up to 24 hours.
Levemir can also be used with rapid-acting insulin, other diabetes products such as tablets, and anti-diabetic effects.
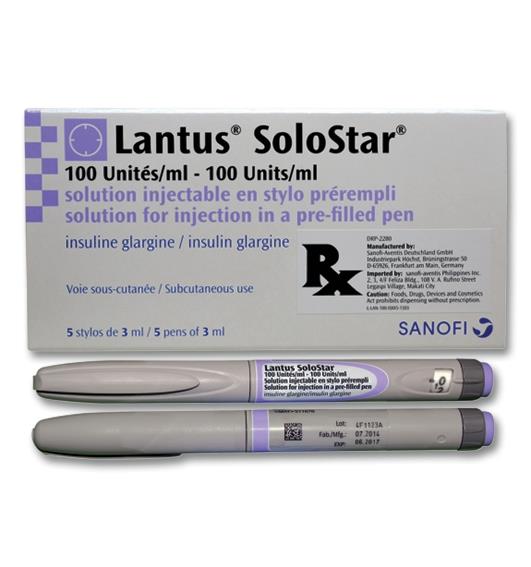
Ensure you are ordering the correct cartridge, as insulin can easily get mistaken amongst the different types of cartridges on the market.
Warnings and Precautions
Do not use Levemir if you are allergic to insulin detemir or any of the ingredients it contains. If you are experiencing hypoglycemia, please discontinue the medication immediately. This medication is not meant for use with insulin pumps.
If the device is damaged, crushed, dropped, or frozen, please discontinue use.
If the medication does not appear colorless or transparent, do not use it.
Your approval to use insulin or dosage requirements may be affected by the following:
– If you have trouble with your liver or kidneys or your thyroid, pituitary, or adrenal glands.
– If you exercise more than regular or have made drastic dietary changes to your blood glucose levels.
– Suppose you are traveling abroad to a different time zone. Your insulin schedule may change as a result.
– If you are experiencing illness, do not stop taking your insulin and consult your doctor if this happens.
– If you experience skin changes at the injection site.
– If you have very low albumin, you will need to monitor your blood sugar levels.
Inform your doctor or pharmacist if you are currently taking or have recently taken any of the medications mentioned below. These medications may affect blood glucose levels and may require an adjustment to your insulin treatment.
Usage
Before Use
– Make sure you are using the correct type of insulin by checking the label.
– Inspect the cartridge, including the rubber plunger.
– Do not use it if it is damaged. This includes the rubber plunger that has been drawn above the white label at the bottom of the cartridge. This could indicate an insulin leakage. Return to the supplier if you find the cartridge is damaged.
– To prevent contamination, always use a new needle.
– Do not share the Levemir Penfill or needles as this can lead to spreading infection.
– Levemir Penfill should only be administered subcutaneously (under the skin).
Always rotate injection sites to avoid changes to the fatty tissue under the skin, such as skin shrinking, thickening, or developing lumps on the skin. Notify your doctor if you are currently injecting into affected areas.
When to Take Levemir?
Constantly adjust your insulin dosage and follow regimen as instructed by your doctor or pharmacist.
Levemir can be used in combination with short- or rapid-acting insulin.
For those with type 2 diabetes, Levemir may be used in combination with other diabetes medications such as tablets or injectable anti-diabetic products.
Your dosage may need to be adjusted if your doctor switches you over to another brand of insulin or has prescribed another medication to be part of your treatment.
How often do you Inject Levemir?
Levemir is typically administered once daily. When used as part of a basal-bolus insulin regimen, Levemir is administered twice daily depending on the patient’s individual needs.
Dosage should be administered at the same time every day.
For patients who require two daily doses, you can administer the second dose in the evening or at bedtime to optimize blood sugar control.
How and Where to Inject Levemir?
Levemir Penfill is only to be injected under the skin. It should never be injected into a muscle or vein.
The best places for injection include the front of the thigh, upper arm, or front of the waist (abdomen). Be sure to rotate injection sites and measure blood sugar levels regularly.
Use the injection technique as advised by your doctor or nurse. Also, refer to the manual.
Keep the needle in the skin for at least 6 seconds and keep the button pushed until the needle has been fully withdrawn. This will ensure the complete delivery of insulin.
Do not refill the cartridge.
Side Effects
Hypoglycemia is the most common side effect when taking insulin which affects more than 1 in 10 people.
Low blood sugar may be caused by injecting too much insulin, skipping a meal or overeating, exercising more than usual, and consuming alcohol.
Symptoms of hypoglycemia may include cold sweats, headaches, increased heartbeat, Illness, impaired vision, drowsiness, nervousness, hunger, cool pale skin, anxiety, confusion, difficulty concentrating, and unusual tiredness.
Warning signs of hypoglycemia may be gradual and include increased thirst, increased urination, nausea or vomiting, feeling exhausted, flushed, dry mouth, or dry skin.
If you experience hypoglycemia, you will need to consume a sugary snack or beverage or glucose tablet. You should always carry hard candy, jelly beans, sugar packets, or glucose tablets around with you just in case. Continue your insulin treatment as usual once your blood sugar levels have stabilized.
Severe hypoglycemia can lead to losing consciousness and can lead to brain damage (temporary or permanent). If you become unconscious and cannot consume sugar orally, you will require someone to give you a glucagon injection, a hormone that will cause your blood sugar to rise. If you do not respond to the glucagon treatment, you will need immediate medical attention at a hospital.
Educate family and friends on what to do if you lose consciousness, such as turning you over to your side if you pass out and not giving you anything orally such as food or drinks, as this might cause you to choke.
Speak to your doctor if you are experiencing consistent low blood sugar levels that result in losing consciousness and requiring glucagon treatment. You may need an adjustment to your insulin treatment (dosage, timing, etc.).
High blood sugar (Hyperglycemia) may occur if: you have not injected enough insulin, skin an insulin dose, ration insulin, eat more than usual, exercise less than expected, get an infection or fever.
Warning signs of hyperglycemia include increased thirst, urination, drowsiness/tiredness, feeling flushed, dry mouth, fruity (acetone) breath, feeling ill (nausea or vomiting), loss of appetite.
If you experience any of the signs of hyperglycemia mentioned above make sure you test your blood sugar levels and urine (for ketones) and seek medical attention immediately.
If not treated, this may lead to a severe condition called insulin ketoacidosis, a build-up of acid in the blood. If untreated, this can lead to a diabetic coma and eventually death.
Allergic reactions are rare and usually affect 1 in 10,000 people. Severe allergic reactions to insulin may occur if an individual is allergic to the insulin or one of its ingredients.