Humalog Cartridges 100 Units/mL Description
Humalog cartridges 100U/mL are filled with insulin lispro, a fast-acting (manufactured) insulin similar in structure to naturally occurring insulin produced by the pancreas in the body. Insulin is a hormone that helps regulate blood sugar levels and the breakdown of food (fats, sugars, and proteins). It promotes the absorption of sugar from the blood into the liver, fat, and musculoskeletal cells.
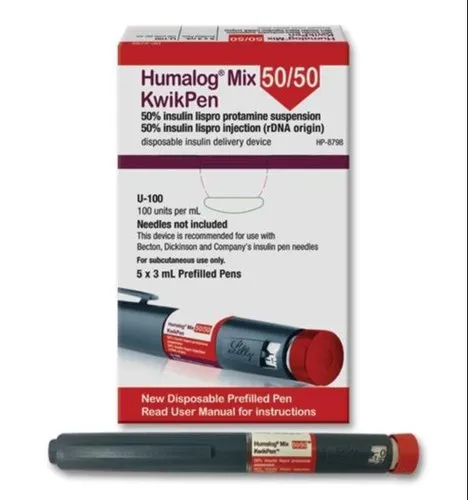
Humalog cartridges are to be used along with Humalog KwikPens (such as the 100 and 200 unit models), which are used by adults and children (over the age of 3) to treat type 1 and type 2 diabetics. Some evidence has shown that Humalog insulin lispro may be effective in preventing diabetic neuropathy.
Ensure you are ordering the correct insulin, as Humulin and Humalog tend to get mixed up with one another.
It effectively helps manage blood sugar levels that typically fluctuate before or after meals. Compared to natural insulin, insulin lispro has a shorter onset delay, meaning you only have to wait a short period before starting your meal.
Warnings and Precautions
Do not use Humalog cartridges if your blood sugar levels are too low (hypoglycemia). If you experience hypoglycemia, be sure to follow your doctor’s instructions on using your insulin medication.
A drop in blood sugar level can be attributed to stress, surgery, exercise, illness, drinking alcohol, or skipping meals.
Do not change your insulin dose schedules without consulting your physician.
Do not use if you have any allergies to its ingredients in the Humalog cartridge.
Do not share your cartridge, syringe, or injection pens with others, even if the needle has been changed. This can lead to the transmission of blood pathogens.
In the case of an overdose which can lead to hypoglycemia. Test immediately and confirm. Whether or not you test your blood sugar levels, it’s essential to consume glucose (i.e., juice, candy, chocolate, etc.) and immediately seek medical attention.
Interactions of Humalog 100iu Cartridge 3ml
If you are taking other medications with Humalog, you may experience symptoms of low blood sugar. Some medicines can block your body’s response to low blood sugar, so you may not experience otherwise severe symptoms such as anxiety, sweating, hunger, blood sugar drops, or headaches.
Medications that can cause complications with insulin include:
– Medicines for fever and pain (salicylates), lisinopril or ramipril
– You may have high blood sugar if you take thiazide, steroids, oral contraceptives, medicines to treat diarrhea, octreotide, thyroxine.
– Be cautious if you take Pioglitazone, which has been reported to cause a heart attack or heart failure.
Usage
Humalog insulin lispro is engineered to provide rapid absorption and shorter onset delay than natural insulin in the body. It begins to work only after 15 minutes of subcutaneous injection and can achieve peak blood levels in 30 to 70 minutes and last up to 5 hours.
Maintaining a consistent meal schedule is advisable when you are taking insulin.
Humalog insulin lispro should be taken 15 minutes before meals or within 20 minutes of starting a meal.
Follow dose amounts and dosing schedule that are advised by your doctor or explained by the pharmacist. Your dosage and plan are individualized based on your specific needs. Your usual dose of insulin may be affected by food selection and exercise level. Other factors that may modify your dosage include pregnancy, other medications, illness, or travel.
Administer the dose within 15 minutes of starting your meal or 20 minutes after starting your meal. Avoid skipping or delaying meals when you are taking insulin.
Humalog Cartridges are used subcutaneously (under the skin). Injection sites are usually the upper arm, abdomen, buttocks, or thigh. Injection should be taken under the skin.
Do not take this injection into muscle or vein.
Change the injection sites regularly to avoid lipodystrophy. Humalog insulin lispro is usually combined with long-acting insulin such as Humulin N (insulin isophane [NPH]) or intermediate insulin.
If you are mixing insulin, be sure to draw the short-acting insulin into the syringe followed by the longer-acting insulin. Mixing should only be done as advised by your physician.
Do not use insulin if it looks thickened, contains particles, or is cloudy. The solution must be clear and colorless.
Missing a dose can lead to high blood sugar levels, which can cause symptoms such as excessive urination, loss of appetite, thirst, fruity smell on the breath, etc. Be sure to take a dose if you know you missed one unless it’s around the same time as your scheduled dose, then continue with your regular schedule. Do not take double the amount to compensate for the missed dose, as this can lead to a drastic drop in blood glucose and be dangerous.
Side Effects
Common side effects associated with the use of Humalog insulin cartridges include injection site reactions, lipodystrophy, hypoglycemia (low blood sugar), and hypokalemia.
The most common side effect is hypoglycemia which is when blood sugar levels are low. This is common among all insulin medications. If this happens, you may also experience increased heart rate, sweating, tremors, weakness, dizziness, blurred vision, confusion/Trouble concentrating, hunger, headache, nausea, drowsiness, seizures (convulsion), shaking, pale skin, skin rashes, nervousness, anxiety, lightheadedness, pain, swelling, redness at the site of injection.
Injection site reactions are also a common side effect that typically includes itching, swelling, and redness at the injection site. Typically these symptoms go away after a few days or weeks. This can sometimes be due to improper injection techniques or impurities in your cleansing products and not the actual medication.
Hypokalemia has been reported in some patients and can happen when there is a decline in potassium levels in the blood. Symptoms of hypokalemia can include tiredness, constipation, weakness, and leg cramps.
Lipodystrophy is a common complication due to subcutaneous insulin use. It may present itself in two forms: lipohypertrophy (an accumulation of fat around the injection site) or lipoatrophy (a localized loss of fat tissue around the injection site).